7 Expert Ways To Design A Treatment Plan Now

Introduction

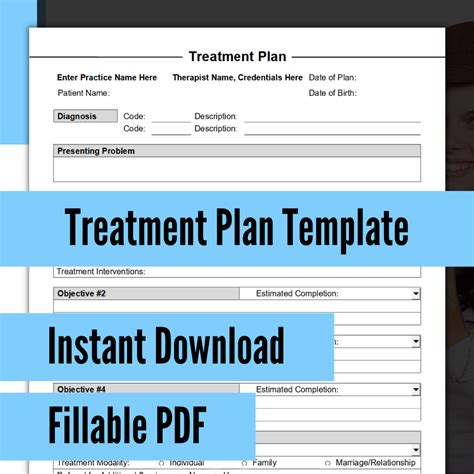
Creating an effective treatment plan is a crucial step in the healthcare journey, whether it’s for managing a chronic condition or addressing a specific health concern. A well-designed plan ensures that patients receive the necessary care, support, and guidance to improve their health and well-being. In this blog post, we will explore seven expert strategies to help you design a comprehensive and personalized treatment plan.
Understanding the Patient’s Needs

Before diving into the treatment plan, it’s essential to thoroughly understand the patient’s unique needs and circumstances. Here’s how you can gather valuable information:
- Medical History: Review the patient’s medical records to identify any previous diagnoses, treatments, and medications. This provides a comprehensive overview of their health journey.
- Symptoms and Concerns: Engage in open communication with the patient to understand their current symptoms, concerns, and goals. Listen actively and ask clarifying questions to gain a deeper insight into their experience.
- Lifestyle Factors: Consider the patient’s lifestyle, including their diet, exercise habits, sleep patterns, and stress levels. These factors can significantly impact their overall health and treatment outcomes.
- Social and Emotional Support: Assess the patient’s support system and emotional well-being. Social factors play a crucial role in their ability to adhere to the treatment plan.
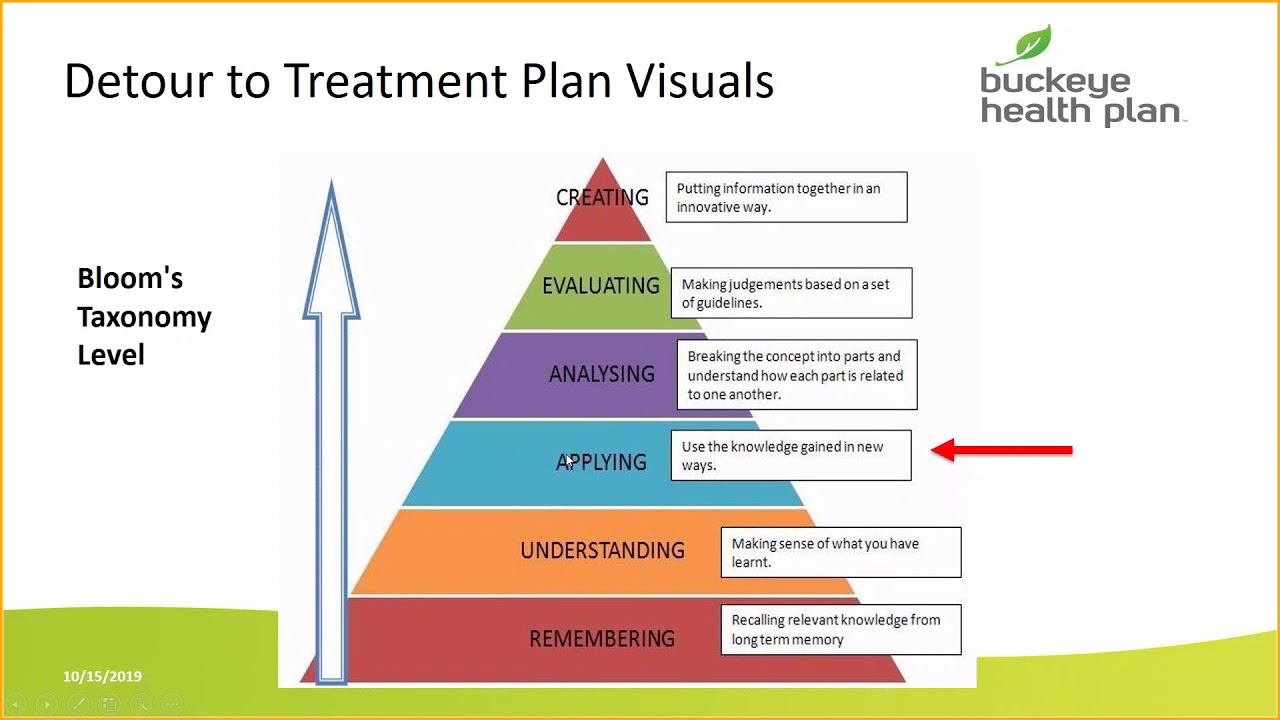
Setting Realistic Goals

Setting clear and achievable goals is a fundamental aspect of treatment planning. Here’s how you can establish realistic objectives:
- Short-Term Goals: Break down the treatment process into smaller, manageable steps. Short-term goals provide a sense of progress and motivation for the patient.
- Long-Term Vision: Work with the patient to define their long-term health goals. This could include achieving specific health milestones or maintaining a certain quality of life.
- Collaborative Decision-Making: Involve the patient in goal-setting to ensure their buy-in and commitment. Discuss different treatment options and consider their preferences and priorities.
Developing a Multidisciplinary Approach
A multidisciplinary approach brings together various healthcare professionals to provide comprehensive care. Consider the following when building a multidisciplinary team:
- Specialist Referrals: If the patient’s condition requires specialized care, refer them to relevant specialists. This ensures they receive expert guidance and treatment.
- Collaborative Care: Encourage open communication and collaboration between different healthcare providers. Regular team meetings can help coordinate treatment and address any concerns.
- Patient-Centered Care: Ensure that the patient remains at the center of the multidisciplinary team. Their input and feedback are essential for a successful treatment outcome.
Personalizing the Treatment Plan

Every patient is unique, and their treatment plan should reflect their individual needs. Here’s how you can personalize the plan:
- Individualized Medications: Prescribe medications tailored to the patient’s specific condition and health status. Consider their medical history, allergies, and potential drug interactions.
- Lifestyle Modifications: Recommend lifestyle changes based on the patient’s preferences and capabilities. These could include dietary adjustments, exercise routines, or stress management techniques.
- Education and Support: Provide educational resources and support to help the patient understand their condition and actively participate in their treatment. Offer guidance on self-care and healthy habits.
Monitoring and Adjusting

Treatment plans are not static; they require regular monitoring and adjustments to ensure effectiveness. Here’s how you can implement this process:
- Regular Check-Ins: Schedule frequent follow-up appointments to assess the patient’s progress and address any emerging issues. These check-ins allow for timely adjustments.
- Data Analysis: Collect and analyze data, such as vital signs, lab results, and patient-reported outcomes. This data provides valuable insights into the effectiveness of the treatment plan.
- Flexible Approach: Be prepared to make adjustments to the plan based on the patient’s response and changing circumstances. Flexibility is key to adapting to their needs.
Utilizing Technology and Resources

In today’s digital age, technology can be a powerful tool in treatment planning. Consider the following:
- Digital Health Platforms: Utilize online platforms and apps that offer convenient access to health information, tracking tools, and support communities. These can enhance patient engagement.
- Telehealth Services: Offer remote consultations and monitoring through telehealth services. This option is particularly beneficial for patients with limited mobility or those in rural areas.
- Research and Evidence-Based Practices: Stay updated with the latest research and evidence-based practices in your field. Incorporate proven strategies into the treatment plan.
Empowering Patients for Self-Care
Empowering patients to take an active role in their self-care is a vital aspect of treatment planning. Here’s how you can encourage self-care:
- Education and Awareness: Provide patients with educational materials and resources to increase their understanding of their condition. Knowledge empowers them to make informed decisions.
- Skill-Building: Teach patients specific skills, such as stress management techniques, pain management strategies, or medication adherence tips. These skills enhance their ability to manage their health.
- Support Groups: Connect patients with support groups or online communities where they can share experiences and receive encouragement. Social support is essential for long-term adherence.
Conclusion
Designing a treatment plan requires a holistic approach that considers the patient’s unique needs, goals, and circumstances. By following these expert strategies, you can create personalized and effective treatment plans that empower patients to take control of their health. Remember, collaboration, flexibility, and a patient-centered approach are key to successful treatment outcomes.
FAQ

How often should I review and adjust the treatment plan?
+
It is recommended to review the treatment plan at least once every 3-6 months or whenever significant changes occur in the patient’s health status. Regular reviews ensure that the plan remains relevant and effective.
What if the patient’s condition deteriorates despite the treatment plan?

+
If the patient’s condition worsens, it is crucial to reassess the treatment plan and consider alternative approaches. This may involve consulting with specialists or exploring different treatment options.
How can I ensure patient adherence to the treatment plan?

+
To improve patient adherence, provide clear and concise instructions, offer support and regular check-ins, and address any concerns or barriers they may have. Building a strong patient-provider relationship is key.
Are there any legal considerations when designing a treatment plan?

+
Yes, it is important to adhere to legal and ethical guidelines when creating a treatment plan. Ensure that the plan is evidence-based, respects patient autonomy, and complies with relevant healthcare regulations.
Can patients have input in the treatment plan design process?

+
Absolutely! Patient involvement is crucial for a successful treatment plan. Encourage open communication, consider their preferences, and involve them in decision-making to increase their commitment and adherence.